Introduction
Prior to the widespread use of Papanicolaou (PAP) smears in the 1950s, cervical cancer was a major cause of death for American women of child-bearing age. Due to early detection and treatment, cervical cancer is now the 14th most common malignancy affecting American women (NCI, 2010a, NCI, 2010b). World wide, cervical cancer is the third most common cancer affecting women (PubMed Health, 2010). The National Cancer Institute estimates that there will be 12,360 new cases of cervical cancer in 2014. Of these, it is projected that 4,020 will die.
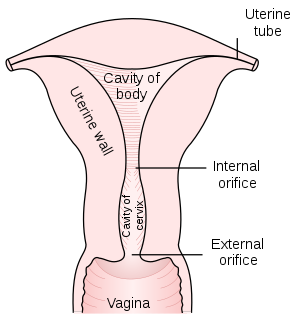
Posterior half of uterus and upper part of vagina. Figure 1167 from Gray’s Anatomy. (Photo credit: Wikipedia)
Anatomy
Uterine anatomy includes (see diagram to the right): the uterus, fundus, cervix, vagina, internal orifice, and external orifice.
Types of Cervical Cancer
Cervical cancers are typed according to the cells they originate from and how they appear under the microscope. The types of cervical cancer are (Cancer.org, 2012).
Squamous cell carcinoma: This is the most common type of cervical cancer. 80 to 90 percent of cervical cancers are squamous cell carcinomas. They most commonly occur in the transformation zone where the exocervix (outer portions of the cervix) meets the endocervix (inner portions of the cervix, including cells in the cervical canal).
Adenocarcinoma: Adenocarcinoma of the cervix has been increasing in frequency over the pas 20 to 30 years. Adenocarcinoma of the cervix arises in the mucous producing glandular cells of the endocervix.
Mixed Carcinoma: Cancer of the cervix can have both squamous and adenocarcinoma characteristics. When this happens, the cancer is said to adenosquamous or mixed carcinomas.
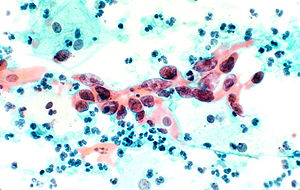
Histological section showing cervical cancer specifically squamous cell carcinoma in the cervix. Tissue is stained with pap stain and magnified x200. Histology Type: Color Slide Source: National Cancer Institute Author: Unknown photographer AV Number: AV-9303-4404 Date Created: March 1993 Date Entered: 1/1/2001 Access: Public (Photo credit: Wikipedia)
Other types of Cancer: Lymphoma, sarcoma and melanoma are most commonly found in other parts of the body, they they can also occur in the cervix.
The Role of the Human Papilloma Virus (HPV) in the Development of Cervical Cancer
The National Cancer Institute (NCI) reports that almost all cases of cervical cancers are cause by HPV (NCI, 2011). Not all women who are exposed to HPV develop cervical cancer. In the majority of women, the immune system is able to destroy the virus. In a small percentage of women, the virus manages to survive inside the cells of the cervix for many years. While inside the cells, the HPV virus is able to cause the cells to become cancerous (Mayo Clinic, 2011).
Pap smears enable doctors to detect cervical cancer in the early stages of development. Because of screening, death from cervical cancer is decreasing. Doctors hope that the HPV vaccine will prevent development of cervical cancer (Mayo Clinic, 2011).
The following risk factors increase the chances of getting cervical cancer (PubMed Health, 2010, NCI, 2012) :
- Having sex at an early age
- Multiple sexual partners
- Having sex with a partner who has multiple sexual partners or engages in high risk sexual activities.
- Women whose mothers took DES (diethylstilbestrol- a drug that was given to prevent miscarriage). This drug was most likely to have been prescribed in the 1960s.
- Compromise of the immune system (HIV/ AIDS and other immune diseases)
- Giving birth to many children
- Smoking cigarettes
- Use of oral contraceptives
- Women who are too poor to have PAP smears
Symptoms
Symptoms of cervical cancer are (PubMed Health, 2010):
- Vaginal bleeding after intercourse or in between periods
- Post-menopausal bleeding
- A continuous, pink, watery, bloody or brown vaginal discharge that may also have a foul odor.
- Periods that last longer and are more heavy than usual
- When cervical cancer is more advanced the following symptoms may occur:
- Fatigue
- Bone fractures
- Back pain
- Heavy vaginal bleeding
- Appetite loss
- Weight loss
- Pelvic pain
- Swelling in one leg
- Leg pain
- Leakage of urine or feces from the vagina
Diagnosis
From 1955 to 1992, deaths from cervical cancer in the U.S. decreased 60 percent, due to early diagnosis and treatment (NCI, 2010b). The PAP smear and pelvic examinations are the mainstays for early detection of cervical cancer. Pelvic examination is a routine part of a woman’s physical exam. During the pelvic exam, the uterus, ovaries and fallopian tubes are evaluated for size, shape, tenderness and the presence of abnormalities. The PAP smear is obtained from the cervix via speculum during a vaginal exam. Ideally, cells from the endocervix should be obtained, in addition to other cervical cell.
Other tests included in the evaluation for cervical cancer are (PubMed Health, 2010, NCI, 2012):
- HPV test
- Endocervical curettage (ECC)
- Colposcopy
- Cone biopsy (to see how far into the cervix the cancer has spread)
The following tests are done to see if cervical cancer has spread to other organs:
- Chest X-ray
- CAT Scan
- Cystoscopy (to see if cervical cancer has spread to the bladder)
- IVP (to see if cervical cancer has spread to the bladder, ureters or kidney)
- MRI
Treatment
Treatment of cervical cancer depends upon the woman’s age, general health status, type of cervical cancer and the extent to which the disease has progressed. The woman’s desire to have children is also a factor in determination of treatment.
Early non-invasive cervical cancer can be treated without surgical intervention. Treatment methods for early cervical cancer include (PubMed Health, 2010):
- Cryosurgery
- Laser therapy
- Loop electrosurgical excision procedure (LEEP)
Prevention
- Prevention of cervical cancer is aimed at elimination of risk factors. The following measures are known to reduce the risk of cervical cancer (PubMed Health, 2010):
- Guardasil: Guardasil is the first anti-cancer vaccine. It is effective against the two most common strains of HPV known to cause cervical cancer. Guradasil has been shown to prevent the development of pre-cancerous lesions of the cervix.
- Use of condoms reduces the risk of HPV infection and genital warts. Women should not have intercourse with a sexual partner who has genital warts.
- Avoid having mutliple sexual partners.
- Do not have sex with partners who engage in high risk sexual activities such as sex with multiple partners.
- Annual pelvic exams and PAP smears should be obtained as soon as a female becomes sexually active. In women who are not sexually active, screening examinations should be start at the age of 20.
Trends
In the U.S. cervical cancer increased slightly until 2000. From 2000 to 2010, incidence decreased slightly for whites and stabilized for blacks and hispanics (NCI, 2010).
References
- Cancer.org. (January 18, 2012). Cervical cancer, what is cervical cancer?
- Mayo Clinic. (June 23, 2011). Cervical cancer, definition.
- National Cancer Institute. (n.d.). Definition of cervical cancer.
- National Cancer Institute. (April 15, 2010a). Cervical cancer screening.
- National Cancer Institute. (November 29, 2010b). Cancer advances in focus, cervical cancer.
- National Cancer Institute. (January 26, 2012). General information about cervical cancer.
- National Cancer Institute. (March 27, 2014). Cervical cancer.
- PubMed Health. (November 17, 2012). Cervical cancer.




